MVR
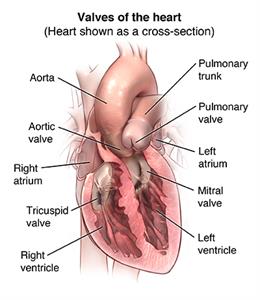
Mitral Valve Repair (MVR) or Mitral Valve Replacement (MVR) are surgical procedures used to treat mitral valve disease, a condition affecting the valve between the left atrium and left ventricle of the heart. The mitral valve controls the flow of blood from the left atrium to the left ventricle, and its malfunction can lead to serious health issues such as heart failure, arrhythmias, or stroke.
Types of Mitral Valve Disease:
- Mitral Valve Regurgitation (MR): The valve doesn’t close properly, causing blood to flow backward into the left atrium.
- Mitral Valve Stenosis: The valve becomes narrowed, restricting blood flow into the left ventricle.
- Mitral Valve Prolapse: A condition where the valve’s leaflets bulge (prolapse) into the left atrium during contraction, which can sometimes lead to regurgitation.
Mitral Valve Repair (MVR) vs. Mitral Valve Replacement (MVR):
1. Mitral Valve Repair:
- Goal: To preserve the patient’s own valve by correcting the structural issues causing the dysfunction.
- Techniques:
- Annuloplasty: Tightening or reinforcing the valve’s ring (annulus) with a ring or band to ensure the valve closes properly.
- Leaflet Repair: Reshaping or removing a portion of the valve’s leaflets to ensure they close properly.
- Chordal Repair or Replacement: Repairing or replacing the chordae tendineae, the string-like structures that anchor the valve leaflets.
- Advantages:
- Preserves the patient’s own valve.
- Lower risk of infection (endocarditis).
- Avoids the need for long-term anticoagulation therapy (blood thinners).
- Generally better long-term outcomes compared to replacement.
2. Mitral Valve Replacement:
- Goal: To replace the diseased mitral valve with a prosthetic valve when the valve is too damaged to repair.
- Types of Replacement Valves:
- Mechanical Valves: Made of durable materials like metal or carbon. They last longer but require lifelong anticoagulation therapy to prevent blood clots.
- Bioprosthetic Valves: Made from animal tissue (usually pig or cow) or donated human tissue. These valves don’t require long-term anticoagulation but may need to be replaced after 10-20 years.
- Procedure: The diseased valve is removed, and the new prosthetic valve is sewn into place.
Surgical Approaches:
Traditional Open-Heart Surgery:
- Requires a sternotomy (opening the chest) and the use of a heart-lung machine (cardiopulmonary bypass).
- Typically used for more complex repairs or when replacement is necessary.
Minimally Invasive Surgery:
- Performed through smaller incisions (mini-thoracotomy) without the need for a full sternotomy.
- May involve robotic assistance or specialized instruments.
- Benefits include shorter recovery time, less pain, and reduced risk of infection.
Transcatheter Mitral Valve Repair (TMVR):
- A less invasive option where a catheter-based approach is used to repair the valve, typically using devices like the MitraClip.
- Often used for patients who are high-risk for traditional surgery.
Recovery and Outcomes:
- Hospital Stay: Typically 5-7 days for open surgery, shorter for minimally invasive approaches.
- Recovery Time: Full recovery can take several weeks to months, depending on the type of surgery and the patient’s overall health.
- Follow-Up: Regular monitoring with echocardiograms and clinical evaluations is crucial to assess valve function and manage any complications.
Risks and Complications:
- Short-Term Risks: Bleeding, infection, arrhythmias, stroke, or complications from anesthesia.
- Long-Term Risks: Valve dysfunction, particularly with bioprosthetic valves that may deteriorate over time, necessitating reoperation.
Considerations for Surgery:
- The decision between repair and replacement depends on factors like the severity of the valve disease, the patient’s overall health, and the likelihood of successful repair.
- Repair is generally preferred when possible due to better long-term outcomes, but replacement may be necessary in cases of severe damage or when repair is not feasible.
Anesthesia
General
————————-
Hospital Stay
7 Days
————————-
Duration Of Operation
5 hours
————————-
